Items filtered by date: December 2021
What Can Cause Gout?

The foot condition that is known as gout is a form of arthritis that affects millions of Americans. It is caused by excess uric acid in the blood, and can happen from genetic reasons, or from eating foods that have high levels of purines. These include shellfish, red meat, or drinks that are made with large amounts of sugar. The pain comes from crystals that lodge in the joints of the big toe, and can cause extreme difficulty in completing daily activities. In severe cases, many patients report they must crawl up the steps as a result of the debilitating pain, and often require immediate medical attention. Additional symptoms of gout can consist of redness and swelling surrounding the affected joints, and there may be large lumps under the skin that are referred to as tophi. These are typically painless, and may develop into chronic bouts of gout if left untreated. Gout is a painful foot condition, and it is strongly suggested that you consult with a podiatrist if you have the beginning signs of joint pain in the big toe.
Gout is a foot condition that requires certain treatment and care. If you are seeking treatment, contact Deborah Rosenfeld from Rosenfeld Podiatry. Our doctor will treat your foot and ankle needs.
What Is Gout?
Gout is a type of arthritis caused by a buildup of uric acid in the bloodstream. It often develops in the foot, especially the big toe area, although it can manifest in other parts of the body as well. Gout can make walking and standing very painful and is especially common in diabetics and the obese.
People typically get gout because of a poor diet. Genetic predisposition is also a factor. The children of parents who have had gout frequently have a chance of developing it themselves.
Gout can easily be identified by redness and inflammation of the big toe and the surrounding areas of the foot. Other symptoms include extreme fatigue, joint pain, and running high fevers. Sometimes corticosteroid drugs can be prescribed to treat gout, but the best way to combat this disease is to get more exercise and eat a better diet.
If you have any questions please feel free to contact our office located in Marlton, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Everything You Need to Know About Gout
Gout, typically found in diabetic patients, is an unusually painful form of arthritis caused by elevated levels of uric acid in the bloodstream. The condition typically strikes the big joint on the big toe. It has also been known to strike the knees, elbows, fingers, ankles and wrists—generally anywhere that has a functioning, moving joint.
The high level of uric acid in a person’s bloodstream creates the condition known as hyperuricema—the main cause of gout. Genetic predisposition occurs in nine out of ten sufferers. The children of parents who suffer gout will have a two in ten chance of developing the condition as well.
This form of arthritis, being particularly painful, is the leftover uric acid crystallizing in the blood stream. The crystallized uric acid then travels to the space between joints where they rub, causing friction when the patient moves. Symptoms include: pain, redness, swelling, and inflammation. Additional side effects may include fatigue and fever, although reports of these effects are very rare. Some patients have reported that pain may intensify when the temperature drops, such as when you sleep.
Most cases of gout are easily diagnosed by a podiatrist’s assessment of the various symptoms. Defined tests can also be performed. A blood test to detect elevated levels of uric acid is often used as well as an x-ray to diagnose visible and chronic gout.
Treatment for gout simply means eliminating symptoms. Non-steroid anti-inflammatory drugs or NSAIDs (Colchicine and other corticosteroid drugs, etc.) will quell the redness, the swelling, and the inflammation. However, managing your diet, lifestyle changes, and using preventative drugs are all helpful toward fully combating the most severe cases.
Those that lead an inactive lifestyle are at a higher risk for gout. Any amount of exercise decreases the probability of repeat encounters with the condition. Reducing your consumption of red meat, sea food, and fructose-sweetened drinks also reduces the likelihood of chronic gout as well.
Ingesting Vitamin C, coffee, and particular dairy products can help with maintaining a healthy lifestyle. There are new drugs out on the market that inhibit the body’s production of uric acid-producing enzymes. However, reducing or eliminating your overall levels of uric acid is the best remedy to ensuring you lead a gout-free life.
Stress Fractures in the Heel

People who are serious about protecting their foot health ought to be familiar with stress fractures. A stress fracture can affect the bones of the feet and lower legs. It occurs typically when a bone develops a crack or break due to repeated pressure, trauma, or impact. One stress fracture to be aware of is the calcaneal stress fracture. This condition affects the heel bone. There is a wide variety of different symptoms that an individual might experience if they develop a calcaneal stress fracture. Notably, one can experience pain underneath the heel. This pain can worsen when the individual is engaged in weight-bearing activities, such as running, walking, or jumping. Individuals who are particularly at risk for this type of stress fracture include runners and ballet dancers. Stress fractures in the heel can be a serious threat to the health of your feet. Do not take chances, contact a podiatrist if you think you have a calcaneal stress fracture.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact Deborah Rosenfeld from Rosenfeld Podiatry. Our doctor can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact our office located in Marlton, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Stress Fractures of the Foot and Ankle
Our bones are important aspects of our body and they are constantly changing. The heavier the workload for a bone, the more likely it is that calcium will be placed in it. When a bone isn’t used often, there won’t be much calcium within it. When stress from repetitive loads prevent the bone from being able to repair itself, cracks will start to form. Stress fractures are defined as cracks in a bone that result from repetitive force, such as overuse.
The most common cause of stress fractures is a sudden increase in intensity and duration of physical activity. For example, if you begin to run long distances without working your way into doing so, you will be more likely to develop a stress fracture.
Common symptoms of stress fractures are pain and swelling near the weight bearing area on the injured bone. When initial x-rays are performed, it is possible that the fracture will not show up. However, once the stress on the area continues, the damage will increase, and the fracture will be severe enough to show up on an x-ray. Certain parts of the foot are more likely to develop stress fractures than others. Areas that typically have these fractures are: the metatarsals, the navicular bone, the calcaneus, tibia, and fibula.
Since women are at an increased risk of developing osteoporosis, they are twice as likely as men to sustain a stress fracture. Additionally, old age causes a decrease in bone mineral density which is why elderly people are also likely to develop these fractures.
It is important for you to be professionally diagnosed by a podiatrist if you suspect you have a stress fracture, because there are other injuries that can easily be mistaken for a fracture. Sprains, strains, shin splints, plantar fasciitis, and Morton’s neuroma can all easily be mistaken for stress fractures in the foot. Your podiatrist will likely ask you a series of questions to determine what type of pain you are experiencing. These questions will help your doctor identify whether you have a stress fracture.
The best method of treatment for a stress fracture is rest. Additionally, a walking boot, cast, or crutches, will help rest the area that is injured. The typical healing time for stress fractures is 4-12 weeks, however this depends on which bone is involved.
Plantar Warts Can Be Treated!
Diabetes and Poor Circulation Often Go Hand in Hand
 People with diabetes can also suffer from peripheral arterial disease (PAD). This is a disease in which elevated blood glucose levels cause your arteries to narrow. A narrowing of the arteries can restrict the flow of blood to the extremities, otherwise known as poor circulation. PAD symptoms include numb or cold feet, intermittent claudication (leg pain that goes away when resting), bluish colorization in the skin of the legs, loss of hair on the legs or feet, brittle toenails and more. One of the more serious symptoms of PAD is an impaired ability to heal wounds and sores, which can be potentially dangerous for the diabetic patient. As a diabetic, it is wise to be under the care of a podiatrist. They will be able to determine if you have PAD with a non-invasive test of the blood flow in your feet called a brachial pressure index test, or ABPI test. If you have been diagnosed with PAD, your podiatrist will be able to help manage your symptoms and help prevent complications from arising.
People with diabetes can also suffer from peripheral arterial disease (PAD). This is a disease in which elevated blood glucose levels cause your arteries to narrow. A narrowing of the arteries can restrict the flow of blood to the extremities, otherwise known as poor circulation. PAD symptoms include numb or cold feet, intermittent claudication (leg pain that goes away when resting), bluish colorization in the skin of the legs, loss of hair on the legs or feet, brittle toenails and more. One of the more serious symptoms of PAD is an impaired ability to heal wounds and sores, which can be potentially dangerous for the diabetic patient. As a diabetic, it is wise to be under the care of a podiatrist. They will be able to determine if you have PAD with a non-invasive test of the blood flow in your feet called a brachial pressure index test, or ABPI test. If you have been diagnosed with PAD, your podiatrist will be able to help manage your symptoms and help prevent complications from arising.
While poor circulation itself isn’t a condition; it is a symptom of another underlying health condition you may have. If you have any concerns with poor circulation in your feet contact Deborah Rosenfeld of Rosenfeld Podiatry. Our doctor will treat your foot and ankle needs.
Poor Circulation in the Feet
Peripheral artery disease (PAD) can potentially lead to poor circulation in the lower extremities. PAD is a condition that causes the blood vessels and arteries to narrow. In a linked condition called atherosclerosis, the arteries stiffen up due to a buildup of plaque in the arteries and blood vessels. These two conditions can cause a decrease in the amount of blood that flows to your extremities, therefore resulting in pain.
Symptoms
Some of the most common symptoms of poor circulation are:
- Numbness
- Tingling
- Throbbing or stinging pain in limbs
- Pain
- Muscle Cramps
Treatment for poor circulation often depends on the underlying condition that causes it. Methods for treatment may include insulin for diabetes, special exercise programs, surgery for varicose veins, or compression socks for swollen legs.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions, please feel free to contact our office located in Marlton, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Causes Symptoms and Treatment for Poor Circulation in the Feet
The purpose of the body’s circulation system is to transport blood, oxygen, and nutrients throughout the body. A reduction of blood to a specific part of the body may cause one to experience symptoms of poor circulation. The most common causes of poor circulation in the feet are obesity, diabetes, and heart conditions such as peripheral artery disease (PAD). Common symptoms of poor circulation include tingling, numbness, throbbing, pain and muscle cramps.
Peripheral artery disease is a common cause of poor circulation in the legs. Symptoms of PAD are cramping, pain or tiredness in the leg or hip muscles while walking or climbing stairs. This pain tends to go away with rest and starts back up when you begin to walk. It is a condition that causes the blood vessels and arteries to become narrow. Although PAD is more common in adults over the age of 50, it may also occur in younger people. A similar condition called atherosclerosis causes arteries to stiffen up due to a buildup of plaque in the arteries and blood vessels.
Blood clots are also a common cause of poor circulation in the feet. Clots may obstruct blood vessels and if they occur in the legs, they may eventually lead to pain and discoloration. This occurrence is commonly known as deep vein thrombosis (DVT) and it may travel to the lungs. Varicose veins are another condition that may lead to poor circulation, and it is caused by incompetence of the valves in the veins. Women who are overweight are prone to developing this condition. Lastly, diabetes, which is correlated with poor blood sugar metabolism may lead to chronic poor circulation. Those with diabetes often suffer from cramping in the legs, calves, thighs and buttocks.
If you are looking for ways to avoid poor circulation there are some tips you can follow. One tip is to avoid sitting for too long. If you plan to sit down for a long period of time, you should try standing up occasionally, to improve your circulation. Another great way to avoid poor circulation is to exercise. Exercise is an excellent way to pump the heart and increase blood flow. Those who suffer from poor circulation should also avoid smoking, reduce their salt intake, and try to lose weight.
If you are experiencing symptoms from poor circulation in your feet, you should consult with your podiatrist to determine the best method for treatment for you. He or she may prescribe medication in addition to recommending specific lifestyle changes to improve your circulation.
Ways Seniors Can Help Prevent Falls

As a person ages, the chance of falling increases along with the repercussions. Some serious dangers that may result from a fall include a broken hip, a broken wrist, or a head injury. Since the bones are thinner and more brittle, healing can take longer. A fall may also affect a senior’s ability to live alone as well as cause chronic pain and depression. A few ways that seniors can prevent falls are by keeping the body active, having their eyes checked for vision problems, and reviewing medications for side effects. In addition, safeguarding the home by removing loose rugs, installing handrails, and improving lighting in hallways or bedrooms is recommended. Other ways to prevent falls are to install grab bars in bathrooms and use a walker or cane for balance. Wearing shoes with non-skid soles can keep you from slipping or sliding on a polished floor. Foot and ankle symptoms like numbness, tingling, and swelling can contribute to a loss of balance or stability. Please visit a podiatrist for foot and ankle strengthening exercises, as well as other information on how to protect yourself from a fall.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Deborah Rosenfeld from Rosenfeld Podiatry. Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in Marlton, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
Ways to Diagnose Achilles Tendon Injuries
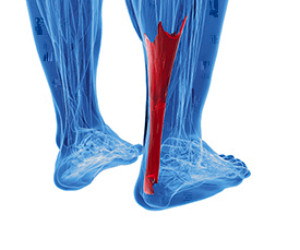
Pain behind the heel is often a sign of an injury to the Achilles tendon. However, finding the exact cause of the pain may require a number of tests. To diagnose an Achilles tendon injury, a podiatrist will start by examining the injured area. A Thompson test involves squeezing the calf to determine the health of the Achilles tendon. The doctor then may ask you to perform a series of physical activities, such as hopping, jumping, or leg lifts, to determine whether the activity causes pain and where it is located. Next, a patient history will be conducted to note any past Achilles tendon injuries or inflammation, as well as a list of your activities. An MRI (magnetic resource imaging) or ultrasound test may also be used to get a detailed look at the tendon or to rule out other injuries or conditions. An X-ray may be used to identify still other factors, such as bone spurs, heel bumps, or stress fractures, that could be causing the pain. If you believe you have injured your Achilles tendon, or are experiencing pain in that area, please visit a podiatrist.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Deborah Rosenfeld of Rosenfeld Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in Marlton, NJ . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.